Free guide to morning sickness and hyperemesis gravidarum care
A unique approach to managing nausea in pregnancy based on the unique challenges faced by today’s mothers

It’s finally here: a new approach to getting out of the nausea and vomiting in pregnancy (NVP) loop. It will guide you through the changes in today’s world that may be exacerbating the normal experience of first trimester nausea for today’s mothers, and what you can do about it.
Catch the replay of the Masterclass here (exclusive for paid subscribers—learn more about what you get with your subscription here), or keep reading for my written deep-dive into morning sickness, NVP and hyperemesis gravidarum.
Morning sickness research compiled by Nikko Kennedy
What we are talking about here spans the normal queasiness and tiredness most women go through at the beginning of their pregnancies (“morning sickness”), through the more extreme diagnoses of nausea and vomiting in pregnancy (NVP) and hyperemesis gravidarum (HG).
I created this originally for women going through severe nausea, vomiting, and fatigue that is causing an inability to go about day-to-day life—and the practitioners who walk with women through this major challenge of pregnancy.
I have seen that women tending towards the more extreme ends of the nausea spectrum are usually stuck in a loop of:
just a few foods that don’t trigger vomiting (most of the time)
just staying in bed/bath/home or wherever there is some feeling of relief
avoiding totally normal places and events such as the car/shower/kitchen/work that have become significant triggers (or out of fear of vomiting in public)
taking medication they don’t truly feel good about taking
And because of these choices, on top of the persistent nausea and frequent vomiting, they are also usually experiencing some (or all) of:
extreme tiredness and sleeping in
restless nights spent tossing and turning, unable to get any deep rest
severe aversions to foods and smells (even ones that were really enjoyable before becoming pregnant)
dramatic mood swings with pervasive feelings of unhappiness, resentment, anger, and guilt/shame
other co-morbidities and complications of health and mental health that may present before, during, or even after the NVP is resolved
I know this because I have walked with many women stuck in this loop.
Through observation and research into the known science of these conditions, I have identified several digestive reset strategies women can use to pop themselves right out of the NVP loop and go on to enjoy their pregnancies, as well as future pregnancies.
These pregnancy digestive reset strategies could also potentially apply to other complications of pregnancy including, but not limited to:
mood disorders
placental insufficiency
miscarriage and recurring miscarriage (as well as secondary infertility)
premature rupture of the membranes
gestational hypertension
IUGR
preterm birth
gestational diabetes
bacterial vaginosis
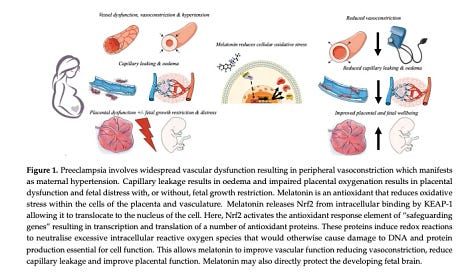
preeclampsia
reducing the likelihood of congenital defects and stillbirth
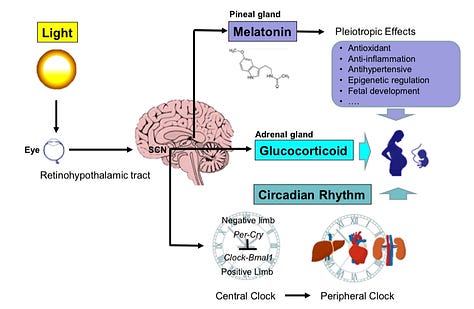
This is really a big deal, and the link is between the circadian rhythm and oxidative stress, which behind the scenes, contributes to the onset and severity of all these conditions.
I hope you will bookmark this page and refer back to it, because when it comes to conventional treatments for NVP (and many other conditions and complaints of pregnancy), options can be quite limited.
For example, as of 2024, “studies on treatments for hyperemesis gravidarum are few, and the certainty of evidence for different treatments is either low or very low.”1 The same is also true of many of the other conditions I listed above, which are also more common in women with a NVP or HG diagnosis.
Keep reading to hear what I have learned, but first, because I know text based learning can be difficult for many, I also offer 1-1 consults for in which we can come up with a personalized lifestyle strategy for you or your client who is suffering from NVP/HG.
Enroll here.
And I also recorded a video class with slides and citations, which you can watch here as a paid subscriber.
Here’s what I have learned about the NVP loop:
All women with HG have NVP, but not all women with NVP have HG
The medical treatments for NVP have limited research to back them up
Many women who get medication for NVP do not feel resolved or satisfied with their treatment even when it reduces their symptoms
Many factors have been speculated and researched as causal factors, but the research tends to come to conflicting results —> however we do know there are a lot of measurable differences in NVP pregnancies including genetic expressions, hormone levels, blood sugar variations, nutritional deficiencies, composition of the gut bacteria and measures of gut motility
Most importantly and why my reset is probably different than anything else you have ever read on this topic: when it comes to actually addressing ALL of these at once, circadian biology and supporting redox and mitochondrial health offer targeted support pathways that are behind all of the current areas of inquiry about the root cause of the problems
Unfortunately, many people (including practitioners) have not been well-educated on circadian biology or redox and so even if they have seen this research, they may not yet understand the implications.
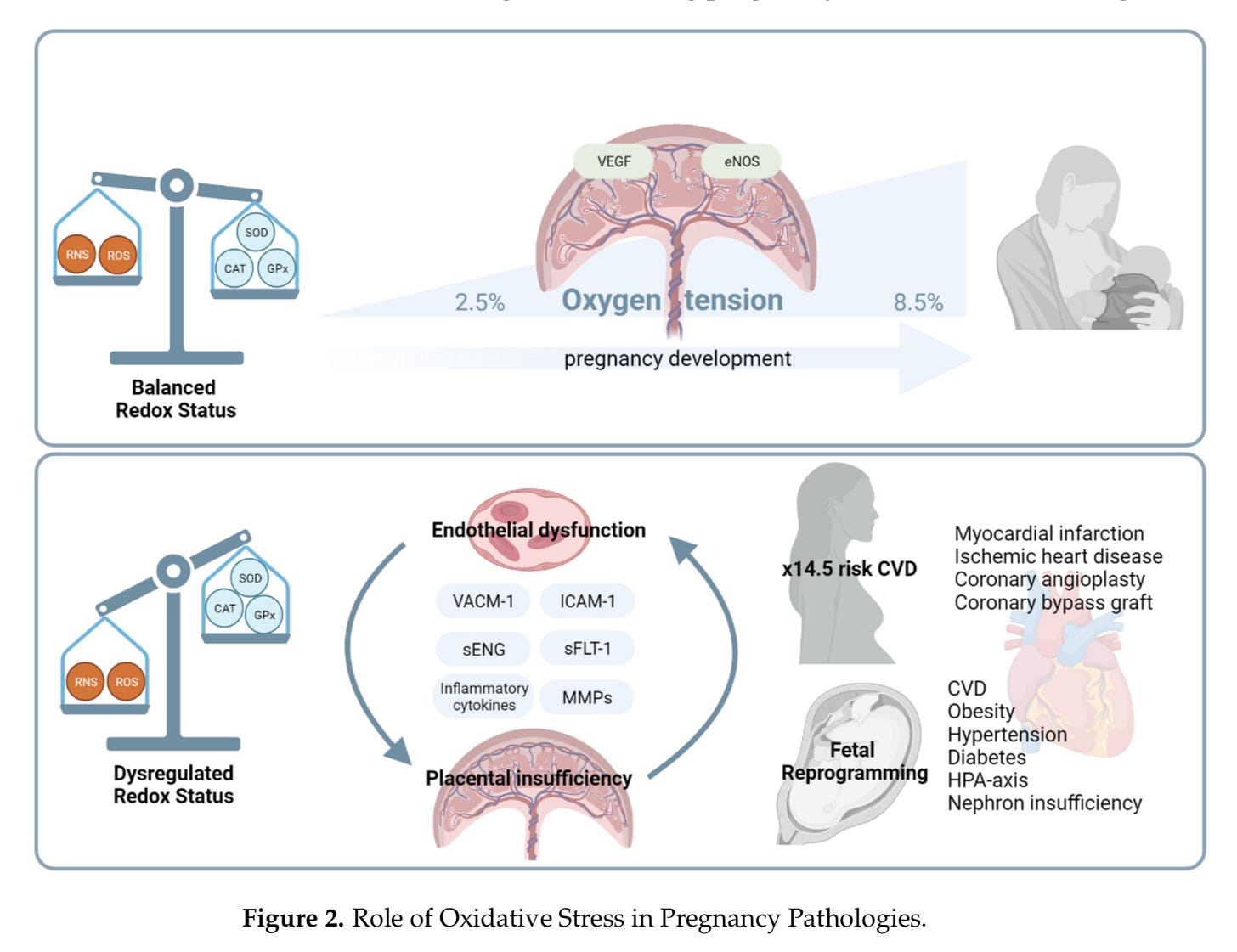
Indeed, the implications are huge particularly because in addition to NVP, oxidative stress is also associated with placental insufficiency, miscarriage, premature rupture of the membranes, gestational hypertension, IUGR, preterm birth, gestational diabetes, bacterial vaginosis, preeclampsia, congenital defects and stillbirth2.
And the good new here is huge, because lifestyle plays such a huge role in redox balance.
Where medications have fallen short when it comes to balancing circadian rhythms (light is stronger than any known drug) and redox (the endogenous antioxidant systems that far outweigh the antioxidants that can come from diet), lifestyle truly shines a light of hope for morning sickness, NVP and even HG.
Redox matters, so I will break this all down and make it very simple and practical.
For a background if this concept of redox is completely unfamiliar, here’s an overview that gives a simple metaphor to understand what is going on:
Redox in normal pregnancies vs pregnancies complicated by hyperemesis gravidarum
Here’s what the redox balance looks like in a normal vs HG pregnancy:
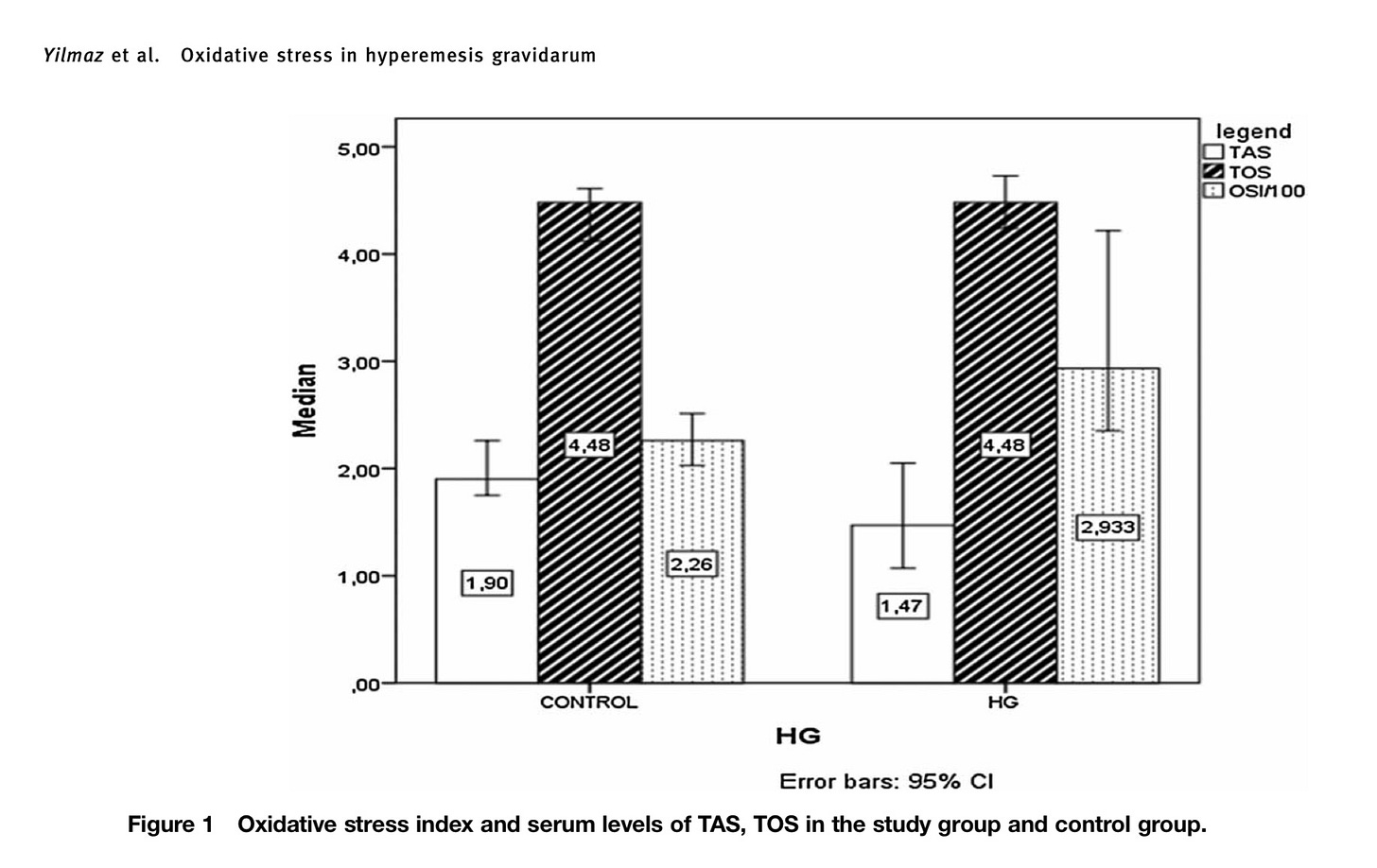
In the above graphic, what I want you to notice is:
The left bars with no shading show the antioxidant capacity
The middle bars with the stripes show the oxidant load
The right bars with the dots show the resultant redox balance
As you can see, the oxidant load (TOS) shown in the middle bars is the same for women with and without HG. Thus, the oxidative stress itself isn’t the problem (remember from my original post about morning sickness that this oxidative stress is part of how the pregnant immune system functions differently, and for those in my practitioner program, you remember redox states are responsible for epigenetic programming and the differentiation of stem cells into unique tissues in pregnancy).
The thing that is different between these groups of women is the decreased antioxidant activity3.
“Hyperemesis gravidarum is an oxidative stress condition, as reflected by increased nitric oxide (NO) and decreased total antioxidant status activity.”
(2018)
I’m going to get into what this means in a minute, but, first, let’s just jump right into the steps to correct this.
The 72-hour pregnancy digestive reset protocol:
Eliminate all artificial light at night, and make sure the sleeping space has a room temperature below 67 degrees Fahrenheit.
Eat 10 grams of high quality protein every waking hour or two (including if you wake at night), with significant inclusion of safe ocean foods like sardines, salmon, shellfish and a variety of seaweeds to taste. Track your intake, adding up to a daily total of 80-100+ grams of protein. Pair proteins with high Vitamin C foods.
Sip warm water with a pinch of mineral salt, a squeeze of lemon or a couple drops of apple cider vinegar, and a few drops of trace minerals (optional) throughout the day.
Sip homemade whey (add a squeeze of lemon if you aren’t a fan of the taste yet):
Have a daily magnesium or epsom salt bath or foot bath or use topical magnesium.
Spend 3 hours (cumulative time, so it can be consecutive but it doesn’t have to be) outside every day touching natural surfaces (recommend earthing shoes if needed based on safety and climate, or put bare hands on trees and plants, garden soil, or the beach). Time touching a natural body of water counts triple. If on bedrest, get grounded sheets instead and make sure the bed is at least 10 feet away from smart meters and wifi routers, and at least 18 inches away from any electrical outlets. This is because nnemfs are linked to problems with redox in the reproductive system4. Since we are trying to increase antioxidant potential (which is another way of saying, free e-), we don’t want anything upsetting the charge inside the body at this time.
With regard to the outside time, early morning and late evening are the best time, when the sun is below 30º of the horizon, because there is little to no UV frequency in the sunlight. The brighter lights of midday can be overwhelming to most women experiencing these symptoms, but if morning light is consumed first, the midday light may be more tolerable. Individual attention is advised.
And a few DON’T items during the reset: NO carbonated drinks, NO refined carbohydrates. Severely limit television watching, cell phone, tablet or computer between dawn and sunset unless for emergency. Aim to reduce exposure to emf fields by with space (at least 18 inches).
Recommendation: also enlist strong social support, personal or professional or both
This reset can be a big shift and big emotions can come up. Enlisting good social support is a must. Many women in this NVP or HG loop carry trauma of having been wronged in the past and may still:
~ believe that they still have not gotten the care they deserve
~ and/or even have deep-seated feelings that they do not deserve a high quality of care
These are two really common ideas I have heard from women with these conditions that need to be acknowledged and resolved so they can overcome the mental blocks they have and move out of the loop.
Without significant emotional work, I rarely see improvement in symptoms, largely because there can be a lack of follow-through in the protocols, but also because of the power of mind and the placebo/nocebo effects.
The emotional work of cultivating resilience is truly a central factor in the ability to follow through with this protocol and get to the next stage of enjoying pregnancy.
I’ve written some ideas that may be helpful here, based on my experiences and training in working with Adverse Childhood EventS (ACES) through the lens of trauma-informed care:
And there is more information about the biological mechanisms of emotional regulation via the vagus nerve and amygdala in the FAQs at the end of this post.
To work with me personally, check out my services at my website. I love walking with women through their pregnancies and am available virtually from Pacific time zone, and in-person in Southern Oregon.
Time commitment for the reset:
With good follow-through, it should only take a few days of this digestive reset protocol for the symptoms to start subsiding. During this time, it’s really important not to get constipated, so taking high quality magnesium orally until the stools are slightly loose can be a helpful tool during the reset. Depending on how long a person has been sick for, it may take more time or less time to get their biology into a fully-functioning state. Sleep quality usually improves dramatically within the first couple of days, and when that is kept up, the rest of the body can begin the healing work. As healing happens, mealtimes will likely eventually consolidate, but if relapse happens—which can happen at the onset of new stressors—it may be a good idea to go back more of the original protocol.
How this pregnancy digestive reset works:
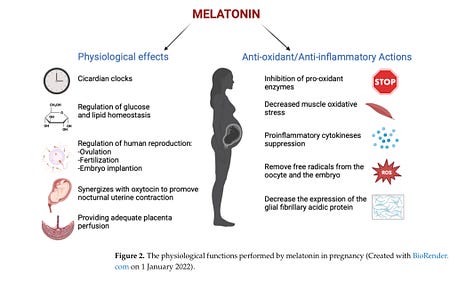
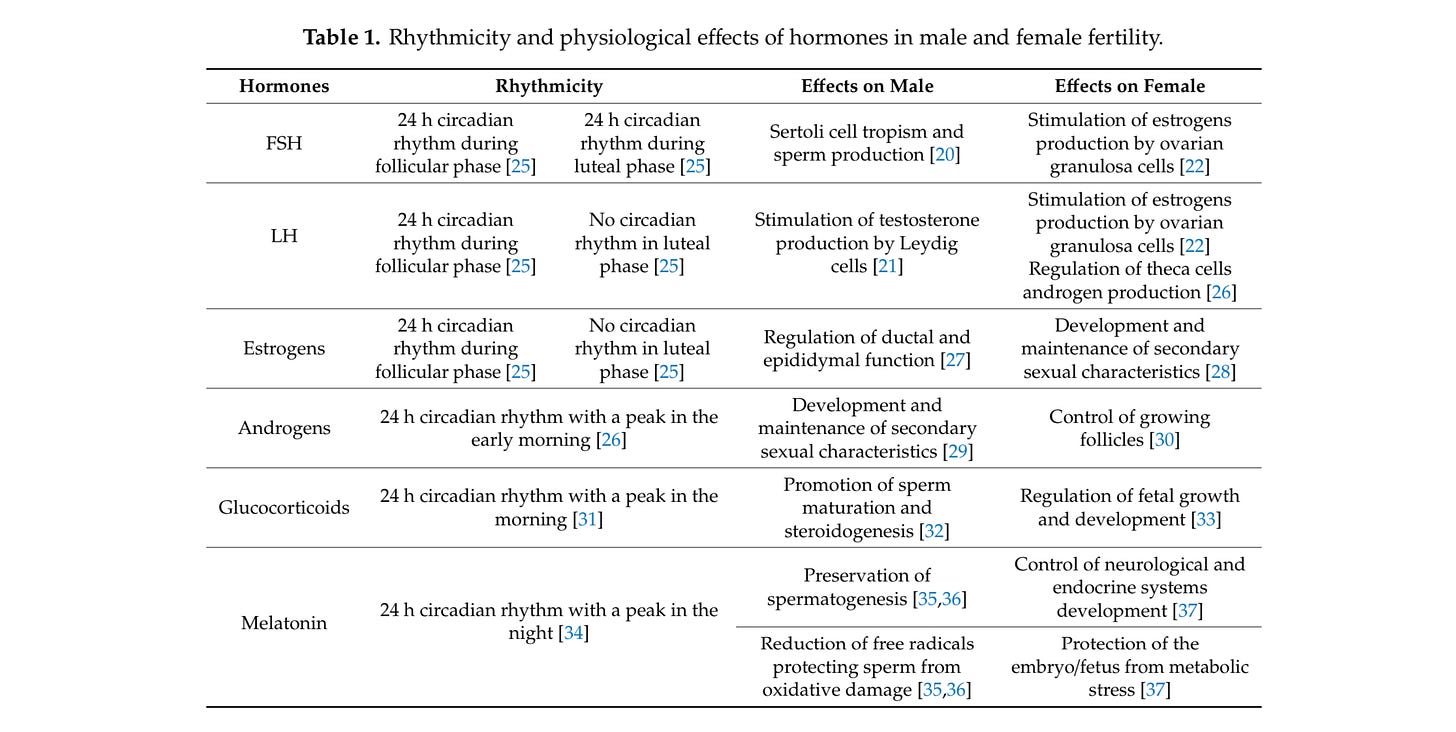
The factors in this reset protocol are based upon my research into optimizing the body’s natural antioxidant protections and the circadian rhythm. The circadian rhythm controls the function/dysfunction of the digestive system5 and the endocrine/hormonal systems and the epigenetic expressions necessary for human reproduction6—all of which have been independently researched in relation to NVP and HG7.
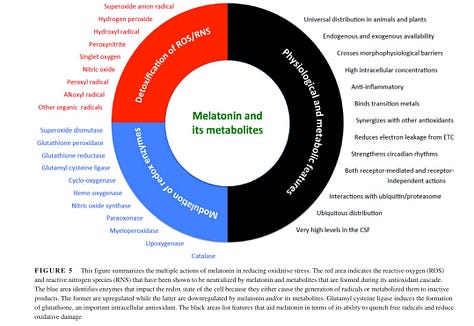
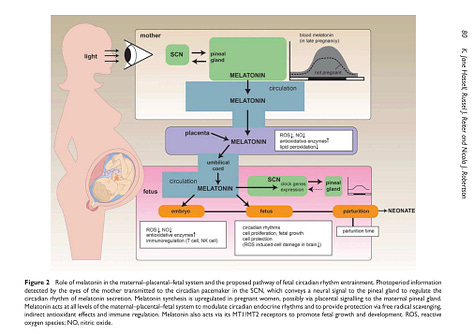
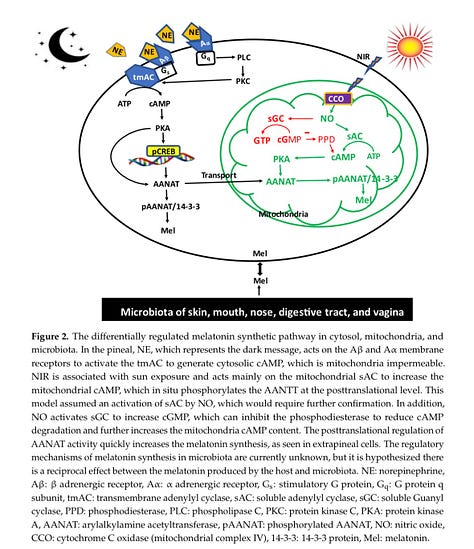
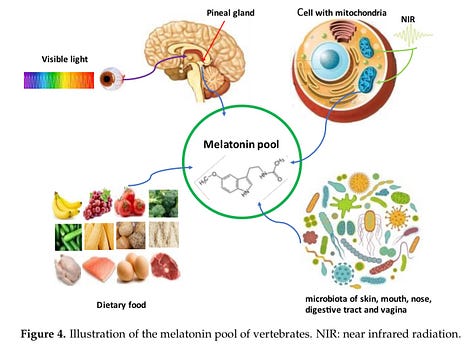
To look at just melatonin, one of the most powerful hormones of the circadian rhythm and also one of the most powerful endogenous antioxidants, we have already seen amazing results in other areas of research.
It seems like we are just waiting for the clinical trial to look at melatonin’s relationship and therapeutic potential in NVP (I can’t find any direct studies—please send them to me here if you know of any!):

Why circadian and quantum biology make sense for escaping the NVP cycle
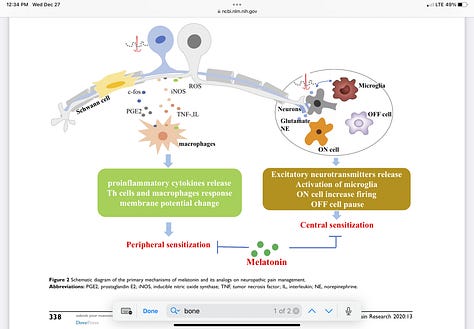
Balancing redox (the balance of oxidant-antioxidant forces) and stabilizing circadian rhythms are the single most actionable insights I can find anywhere that relate to why NVP happens to some women and not others8. This seems especially so when we consider that the circadian rhythm also controls the release of the endogenous antioxidants, particularly melatonin, which in turn regulates glutathione9 and bilirubin and so many other aspects of our antioxidant biology:
“In the present study, we found that oxidative stress in Hyperemesis Gravidarum (HG) is associated with reduction of antioxidants rather than with an increase of oxidants.“
(2015)
The best antioxidants for pregnancy
The main antioxidants to know about for pregnancy are:
melatonin
glutathione
bilirubin<>bilverdin
free electrons from the Earth and/or grounded sheets
the amino acids tryptophan, methionine, histidine, lysine, cysteine, arginine and tyrosine
Vitamins C, D, and E
And, when people have looked into diets that seem to protect against NVP, we see those diets also include the elements above.
What we are looking for is a high-protein (particularly, high meat and seafood), high-antioxidant diet rich in fresh water, low in refined carbohydrates, and absent of carbonated beverages and other sweet drinks10:
“A diet rich in eggs, milk, seafood and unprocessed poultry and animal meat may be a protective factor against HG, while a diet high in beverages may be detrimental to HG.”
(2023)
Melatonin
Melatonin is my go-to starting point for redox work in pregnancy because there are so many ways to boost the pool of melatonin, and because it is highly researched and has proven so beneficial for pregnancy. If you want to learn more about this, please go watch the replay of my Circadian Pregnancy workshop and if you want to understand melatonin from both the circadian and quantum biologic standpoints for the perinatal period, join my Practitioner learning program. Melatonin is more powerful than any of the known dietary antioxidants and everyone can make it themselves.
Glutathione and bilirubin
Glutathione and bilirubin11 are a complimentary pair, with glutathione protecting water-soluble tissues and bilirubin protecting lipid-based membranes12.
It is highly likely that all of the biological activities of bilirubin have yet to be exhaustively explored, and thus we can expect further clinical discoveries about this evolutionarily old molecule into the future.
(2020)
To understand glutathione production better, read my Folate series, and to understand bilirubin better, take my Quantum Newborn Jaundice course.
Earthing as an antioxidant
Earthing has been shown to have near instantaneous affects on the electrical charge in the body, with continued reduction in inflammation (which is another word for oxidative stress in the immune system) seen at 3+ hours and great results seen for grounded sleep environments. Grounding (along with infrared light exposure from sunlight) can also support the body’s internal hydration system, which may be particularly helpful for combatting the dehydration common to NVP. Read these two posts to understand Earthing/Grounding better:
Vitamins C, D, and E
Dietary antioxidants, of course, are a normal part of nutritional advice, however mixed results have been seen with antioxidants like Vitamins C and E in clinical trials13.
“At present, vitamins C and E are usually chosen as antioxidants during pregnancy. Vitamin C can scavenge free radicals in the aqueous phase, vitamin E can prevent LP in vivo, and both can protect against OS. These antioxidants could improve OS, and reduce the risk of the pregnancy disorders associated with OS, such as abruptio placentae and preeclampsia with a low baseline antioxidant status. However, these antioxidants have certain limitations. Firstly, in some conditions, supplementation with vitamin C and vitamin E cannot reduce the risk of preeclampsia, prevent preeclampsia in women at risk, or reduce the pregnancy-associated hypertension; Secondly, supplementation with vitamin C and E during pregnancy has been associated with an increased risk of gestational hypertension, higher stillbirth rate, premature rupture of membranes, and an increased prevalence of babies born with a low birth weight.”
(2017)
This is why I think endogenous antioxidant support14 of melatonin, glutathione, bilirubin and Vitamin D photosynthesis PLUS dietary protein and antioxidant Vitamin foods (not supplements) in palatable doses, make a better antioxidant foundation than supplements of any of the above.
Working all the angles from a natural standpoint allows the body’s own senses to make the choices. In NVP, the sense of smell and taste can be significantly altered, and honoring that while also guiding those senses in a healthier direction is going to be part of the healing process. Women who do heal from NVP usually end up in a better physical/emotional/spiritual state than they were before falling pregnant in the first place.
Thus, while not yet extensively researched, there could be an interrelationship between the collective antioxidant activities of glutathione, vitamin D, and melatonin.
(2022)
For preventing anemia, which may be more likely in women in the NVP loop, Vitamin C, in addition to being an antioxidant, is also helpful for helping the body assimilate the iron in food. For more about this, read my post Boost iron without boosting iron, which is all about taking a more complete view of iron metabolism in anemia than focusing on increasing intake alone.
And Vitamin D will be produced in response to the UV light in this protocol as well as from the eggs, seafood, and pastured meats depending on the time of year and individual history and ancestry. For detailed explanations of safe sunbathing techniques to go along with the grounding, read my post about building a solar callus and about the need for UV light as not only a source of UV light, but also as a neuroendocrine regulator.
Since intense sunlight can be painful in women with NVP, midday exposure may be too intense until high-quality sleep and morning sunlight exposure have stabilized in the routine.
To understand the scope of lack of sunlight on women’s reproductive health, you will also want to subscribe to my Pro tier and watch Lesson 07 in The Circadian and Quantum Childbearing Year practitioner learning program.
Antioxidant amino acids
Of the antioxidant amino acids, tryptophan, in particular, has been investigated for its potential to improve pregnancy outcomes through its very complicated antioxidant cascade (including its role as precursor to melatonin itself, which in turn has it’s own powerful antioxidant cascade).
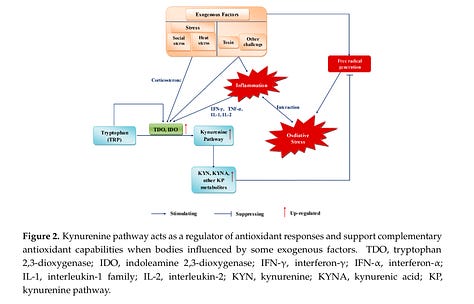
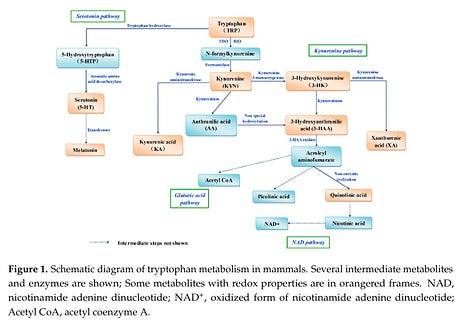
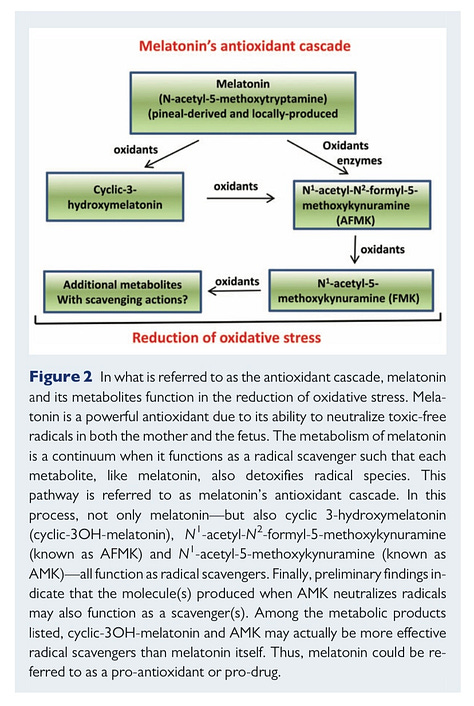
In simple terms, what it means when something has an antioxidant cascade is that it can go through multiple chemical transformations, and each time it releases electrons (e-) that the body can use to balance redox reactions and counteract oxidative stress.
There are other amino acids with antioxidant potential, too, and this is one of the aspects of a high-protein diet I think most people (even proponents of) have been overlooking.
FAQs
I’ve heard hyperemesis gravidarum is a genetic condition. What do you think about that?
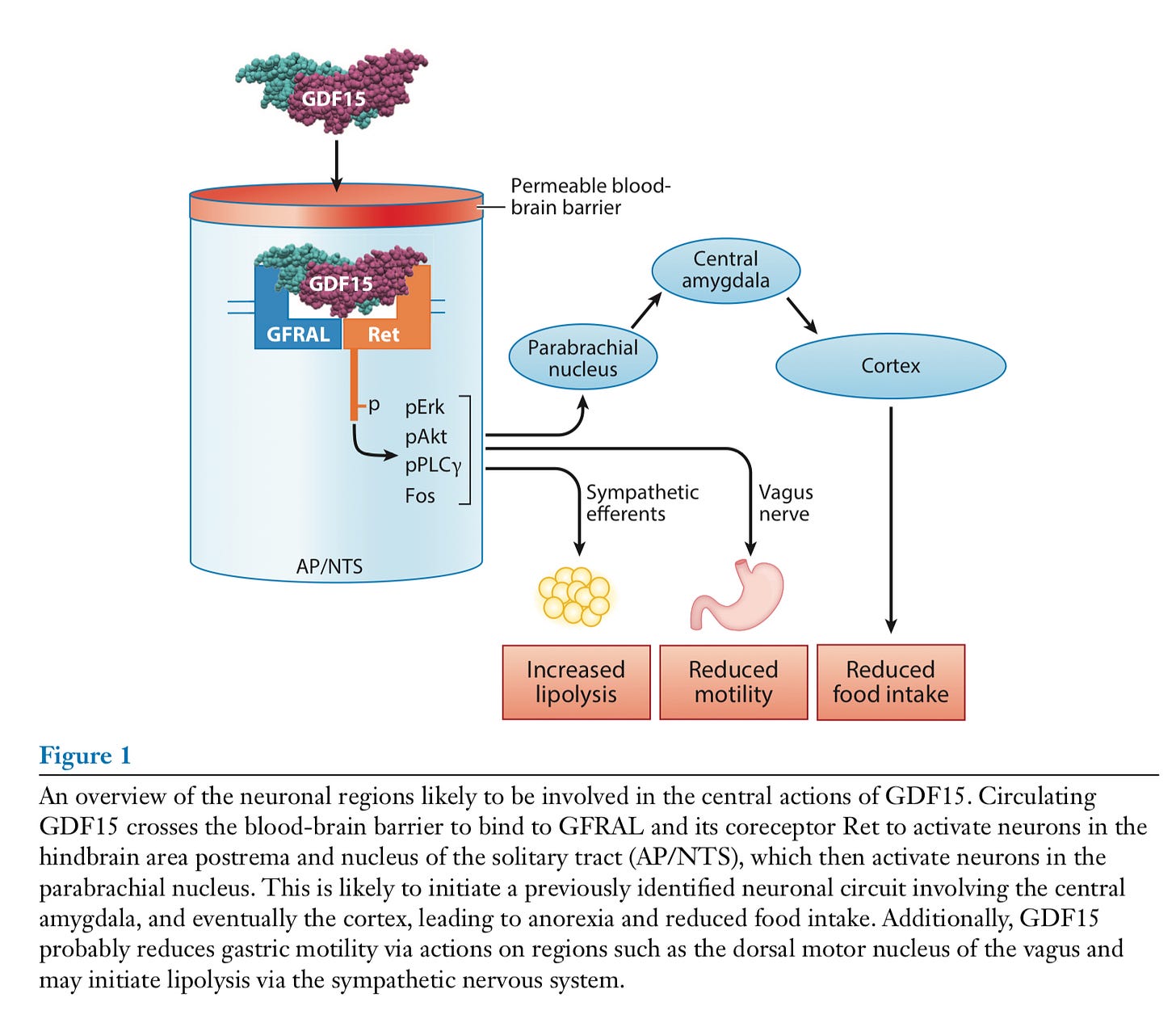
Studies have linked HG to elevated levels of GDF15-GFRAL and we also know there are genetic polymorphisms that have a tendency toward other health conditions (particularly cancers) where this pathway is involved.
However, the root cause of this has not been well researched15 because it is unethical to study humans in this way and:
“The overall role of the GDF15-GFRAL pathway in the evolution of a normal human pregnancy and in the developing fetus and neonate is unclear and difficult to resolve. This is because the robust placental GDF15 expression and the marked elevation of serum GDF15 levels in human pregnancy do not appear to be reflected in the mouse.”
(2021)
What we do know is that GDF15 levels change in response to the cell danger pathways and are interconnected with the emotional centers of the brain and body (such as the amygdala and vagus nerve).
This is part of why my digestive reset protocol asks women to seek very strong social or professional support, not only for the physical aspects, but for creating an atmosphere of emotional safety and the cultivation of resilience, which seems to be a deep root cause challenge to regulating the many factors involved in the NVP loop.
If you think about it, it makes sense that when someone feels unsafe, the body prioritizes survival “fight, flight, freeze, fawn” behaviors and suppresses the seeking of food, positive and healthy social interaction, new experiences and the other things that get suppressed in the spectrum of morning sickness, NVP, and HG.
It also makes sense that certain families may have prioritized survival behaviors over thriving behaviors based on generational trauma.
Finally, the other connection I find really interesting about GDF15 is the most likely medication that will be recommended to women who have this issue is a medication that also targets a redox pathway—pointing back to my thesis here that working towards a balance between the endogenous and exogenous antioxidants and the oxidative stress load is very valid for addressing morning sickness.
I’ve heard hyperemesis gravidarum is caused by nutritional deficiencies. What do you think of that?
Yes, nutritional deficiencies seem to be associated with HG, and that is part of why eating a high-quality, high-protein diet is so key to restoring balance.
I highly recommend reading my Folate series to understand the specific nutrients that best support circadian rhythmicity and healthy redox.
There are a lot of co-factors involved and many of the supplemental vitamin therapies seem to work for some women but miss the mark for others.
Part of that unpredictability will be due to individual differences in intake and burn-rates of co-factors besides the individual vitamins.
You may also be interested in checking out Lily Nichols’ book Real Food for Pregnancy and learning about the Brewer Diet for Pregnancy.
I’ve heard hyperemesis gravidarum is caused by poor blood sugar regulation. What do you think of that?
Yes, insulin issues and problems with blood sugar regulation can appear with HG. This is where it is really interesting that metformin, a diabetes drug that targets redox, mitochondria and glucose metabolism, is being explored as a treatment.
Again, metabolism is regulated by the circadian rhythm and most people are consuming so much excess artificial light (combined with a lack of sunlight, low vitamin D, and inadequate minerals and nutrients), that their cortisol is significantly higher than it should be and coming at the wrong times—this upsets the entire endocrine system, including the digestive hormones like insulin and leptin (which are already known to function differently in pregnancy than other life stages).
Check out my Cortisol series for more about how misunderstood cortisol is as a hormone.
When circadian disruption happens and food signals are not timed with the light signals, blood sugar problems are more likely.
Also, people tend to eat all around the clock and not to prioritize a high-protein, savory breakfast, which would help stabilize both their circadian rhythm and their blood sugars across the day.
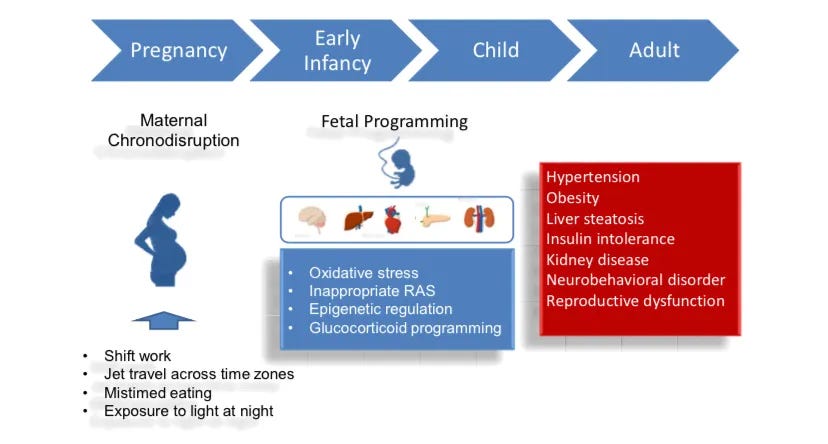
The deck is really stacked against women having healthy metabolisms in pregnancy in the modern environment unless they make significant effort to care for their circadian rhythms and the circadian aspects of digestion.
I’ve heard hyperemesis gravidarum is caused by hormone imbalances. What do you think of that?
Yes, hormone imbalances seem associated with HG.
The thing most advice around hormonal imbalances neglects is the fact that the circadian rhythm regulates the hormones, including the reproductive hormones.
That is why I included a deep reset of the circadian rhythm in this protocol.
In particular, most of the reproductive hormones are released at the end of the rest cycle (this is why getting outside first thing in the morning on a daily basis is so important not only for setting the circadian rhythm and not only for infrared and photobiomodulation, but also for supporting the hormones of fertility).
What do you think of the available medical treatments?
If you have an official diagnosis and are being prescribed treatment, I recommend you share this information with your provider and see if they think any of these steps could be helpful for your unique situation and if they would be compatible with the treatments you are taking.
Based on what I have heard from the women who have tried them, the hydration IV’s can be really helpful (life-saving, even) for severe situations.
The anti-vomiting medications can work, but most women I have spoken with about them report feelings of inadequacy and frustration that they didn’t have a way at getting to the root cause of the vomiting issue (and truly, the constellation of symptoms surrounding the vomiting) and that they really wished they had a way of healing themselves without medication.
More questions? Drop them in the comments.
Resources to support this digestive reset for pregnancy:
Here’s a shopping list for ideas of what to have on hand: Nikko’s Early Pregnancy Protein Food List
Get the free Dminder app and use it to time safe outdoor exposure to the natural sunlight without getting sunburned during the recommended 3+ hours of earthing in this reset. Ideally, outdoor time will be divided into three or four categories to get the maximum benefit from all types of solar exposure:
Early morning light (UV Index 0 primes the circadian rhythm and the skin, giving up to SPF 15 protection later in the day)
Mid-morning light (UV Index 1-3 continues to prime the circadian rhythm and begin activating the neuroendocrine processes through the skin)
Overhead sunlight (UV Index 4+ is what allows the body to synthesize Vitamin D)
Evening light (UV Index 0 is what will boost collagen production to heal any damage from the UV exposure earlier in the day and wind the circadian rhythm down for sleep)
Candles and moonlight are the gold standard for nightlights, but aren’t the most convenient or practical. Check out which nightlights are my favorite (and other helpful circadian and quantum lifestyle products):
Summary:
Severe nausea and vomiting in pregnancy not only interferes with the enjoyment of pregnancy, but can also lead to adverse outcomes for mother-baby.
So far, no one has come up with a universal solution to this issue, but by cross-referencing the latest in circadian and redox biology as well as a trauma-informed social care approach, the steps outlined here present a unique strategy that may support resolution of the underlying mechanisms that interfere with redox and the circadian digestive system in women with severe nausea and vomiting in pregnancy.
Want to learn more or work up a custom plan? Contact me about a 1-1 consult or for more information about a paid subscription to Brighter Days, Darker Nights.
DISCLAIMER: The author is not a medical professional, nutritionist, dietician, therapist or any kind of licensed professional. All material contained in this post is for informational purposes only, and is not guaranteed to be free of errors or omissions in reporting. It has not been evaluated by any medically accredited organization, and is not intended to replace medical advice offered by physicians or other qualified health care providers, or to be used to diagnose, treat, or prevent any type of disease or medical condition. Readers are encouraged the confirm the information with other sources. Before beginning any significant change in lifestyle, or for questions about the diagnosis and treatment of any health-related conditions, it is advisable to see the advice of a licensed healthcare professional. Any application of the material provided is at the reader’s discretion and is the reader’s sole responsibility. The author will not be liable for any direct, indirect, consequential, special, exemplary, or other damages arising therefrom.
Vinnars, M. T., Forslund, M., Claesson, I. M., Hedman, A., Peira, N., Olofsson, H., Wernersson, E., & Ulfsdottir, H. (2024). Treatments for hyperemesis gravidarum: A systematic review. Acta obstetricia et gynecologica Scandinavica, 103(1), 13–29. https://doi.org/10.1111/aogs.14706
Toboła-Wróbel, K., Pietryga, M., Dydowicz, P., Napierała, M., Brązert, J., & Florek, E. (2020). Association of Oxidative Stress on Pregnancy. Oxidative medicine and cellular longevity, 2020, 6398520. https://doi.org/10.1155/2020/6398520
Beyazit, F., Türkön, H., Pek, E., Ozturk, F. H., & Ünsal, M. (2018). Elevated circulating nitric oxide levels correlates with enhanced oxidative stress in patients with hyperemesis gravidarum. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology, 38(5), 668–673. https://doi.org/10.1080/01443615.2017.1383371
Santini, S. J., Cordone, V., Falone, S., Mijit, M., Tatone, C., Amicarelli, F., & Di Emidio, G. (2018). Role of Mitochondria in the Oxidative Stress Induced by Electromagnetic Fields: Focus on Reproductive Systems. Oxidative medicine and cellular longevity, 2018, 5076271. https://doi.org/10.1155/2018/5076271
Voigt, R. M., Forsyth, C. B., & Keshavarzian, A. (2019). Circadian rhythms: a regulator of gastrointestinal health and dysfunction. Expert review of gastroenterology & hepatology, 13(5), 411–424. https://doi.org/10.1080/17474124.2019.1595588
Sciarra, F., Franceschini, E., Campolo, F., Gianfrilli, D., Pallotti, F., Paoli, D., Isidori, A. M., & Venneri, M. A. (2020). Disruption of Circadian Rhythms: A Crucial Factor in the Etiology of Infertility. International journal of molecular sciences, 21(11), 3943. https://doi.org/10.3390/ijms21113943
Liu, C., Zhao, G., Qiao, D., Wang, L., He, Y., Zhao, M., Fan, Y., & Jiang, E. (2022). Emerging Progress in Nausea and Vomiting of Pregnancy and Hyperemesis Gravidarum: Challenges and Opportunities. Frontiers in medicine, 8, 809270. https://doi.org/10.3389/fmed.2021.809270
Yilmaz, S., Ozgu-Erdinc, A. S., Demirtas, C., Ozturk, G., Erkaya, S., & Uygur, D. (2015). The oxidative stress index increases among patients with hyperemesis gravidarum but not in normal pregnancies. Redox report : communications in free radical research, 20(3), 97–102. https://doi.org/10.1179/1351000214Y.0000000110
Reiter, R. J., Mayo, J. C., Tan, D. X., Sainz, R. M., Alatorre-Jimenez, M., & Qin, L. (2016). Melatonin as an antioxidant: under promises but over delivers. Journal of pineal research, 61(3), 253–278. https://doi.org/10.1111/jpi.12360
Cheng, W., Li, L., Long, Z., Ma, X., Chen, F., Ma, L., Zhang, S., & Lin, J. (2023). Association between Dietary Patterns and the Risk of Hyperemesis Gravidarum. Nutrients, 15(15), 3300. https://doi.org/10.3390/nu15153300
Vítek L. (2020). Bilirubin as a signaling molecule. Medicinal research reviews, 40(4), 1335–1351. https://doi.org/10.1002/med.21660
Sedlak, T. W., Saleh, M., Higginson, D. S., Paul, B. D., Juluri, K. R., & Snyder, S. H. (2009). Bilirubin and glutathione have complementary antioxidant and cytoprotective roles. Proceedings of the National Academy of Sciences of the United States of America, 106(13), 5171–5176. https://doi.org/10.1073/pnas.0813132106
Xu, K., Liu, H., Bai, M., Gao, J., Wu, X., & Yin, Y. (2017). Redox Properties of Tryptophan Metabolism and the Concept of Tryptophan Use in Pregnancy. International journal of molecular sciences, 18(7), 1595. https://doi.org/10.3390/ijms18071595
Minich, D. M., Henning, M., Darley, C., Fahoum, M., Schuler, C. B., & Frame, J. (2022). Is Melatonin the "Next Vitamin D"?: A Review of Emerging Science, Clinical Uses, Safety, and Dietary Supplements. Nutrients, 14(19), 3934. https://doi.org/10.3390/nu14193934
Breit, S. N., Brown, D. A., & Tsai, V. W. (2021). The GDF15-GFRAL Pathway in Health and Metabolic Disease: Friend or Foe?. Annual review of physiology, 83, 127–151. https://doi.org/10.1146/annurev-physiol-022020-045449







I'm a bit hesitant to ask another question, given the time and effort your generous responses require. However, I'm curious about your opinion on IR light lamps for those of us who might miss out on natural infrared exposure some days and happen to have a lamp at home. 🏠 🚨
Nikko, I noticed no mentions on Vitamin B6 or CoQ10 which are commonly repeated recommendations I see given by practitioners. I was hoping you’d address those in the FAQs perhaps guiding us into why you think they may or may not be useful.
Oh, and last thing, I clicked a couple of links that don’t work just so you know.
(As I was reading, I was frenetically clicking all links and saving as bookmarks for later 😆😅)